Gm case (20 years)
GENERAL MEDICINE
20-12-22
This is an online E log book to discuss our patient's de-identified health data shared after taking his /her/guradian's consent.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs in the comment box below.
DATE OF ADMISSION :19-12-22
A 20 old male student from miryalaguda came to OPD with
CHIEF COMPLAINTS : backache since 1 day, neck pain since 2 days.
HOPI:patient was apparently asymptomatic 3 days back, then he developed fever which is inscidious in onset, low grade, intermittent not relived on medication.
He developed neck pain 2 days back which is dragging type and was inscidious in onset, gradually progressive, non radiating and no relieving and aggrevating factors, which was not associated with vomitings, giddiness loss of consciousness.
Back pain since 1 day which was sudden in onset in the lower lumbar region and pricking type, continuous, no aggrevating and relieving factors
-no h/o burning micturition, decreased urine output
Past history:
At 12 yrs of age he was found to have severe anemia and underwent blood transfusion
Not a known case of Diabetes, HTN, asthama, epilepsy, TB.
Personal history:Diet mixed, appetite normal, sleep adequate, bowel-regular, micturation-history of haematuria yesterday evening.
No addictions.
FAMILY HISTORY:
Consanguinous marriage
GENERAL EXANINATION :
On examination patient is conscious cooperative and coherent.,
Moderatively built and nourished.
Pallor - present, icterus - present, no cyanosis, no clubbing, no lymphadenopathy, pedal edema.
Vital signs :
Pulse rate - 98beats/min
Resp rate:18 cycles/min
Blood pressure:120/80,
GRBS:152mg/dl
Temperature-afebrile.
SYSTEMIC EXAMINATION :
CVS:s1, s2 heart sound heard, no murmurs.
RESPIRATORY SYSTEM:
Bilateral air entry present
Position of trachea:central,vesicular breathe sounds heard.
CNS:
NAD and higher motor functions intact.
PER ABDOMEN:
INSPECTION:Umbilicus is central and inverted.
No engorged veins and scars seen.
PALPATION :
All inspected findings are normal.
No tenderness felt, spleen-palpable.
PERCUSSION:
No free fluid.
CLINICAL PICTURES:
PROVISIONAL DIAGNOSIS :
Hemolytic anemia.
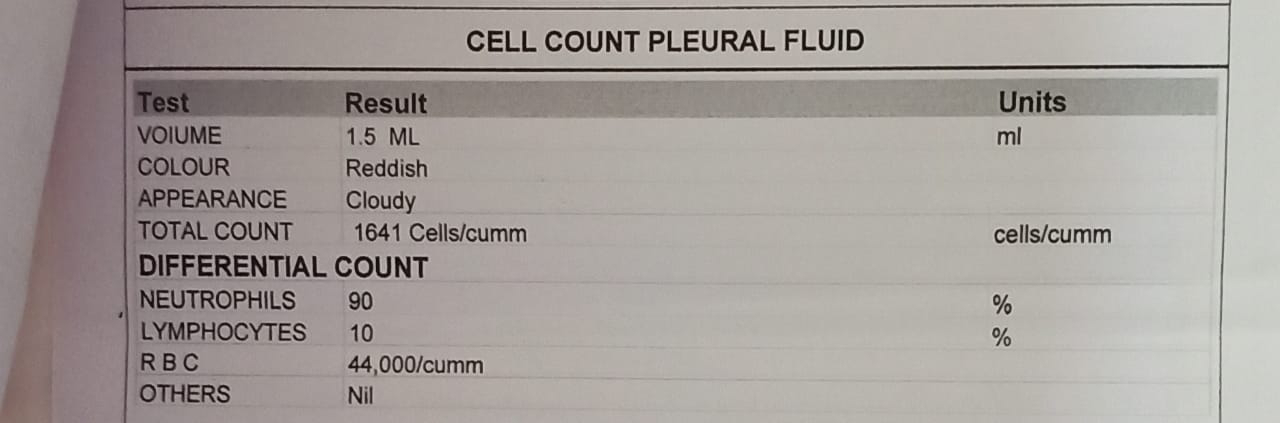
INVESTIGATIONS:







Comments
Post a Comment